The New Technique That May Kill Cancer

Cancer is arguably the largest killer on the planet. It is debilitating disease – and while we currently have some treatment options, we are yet to find a cure.
This is something that very simply needs to be addressed – and recent research has a breakthrough.
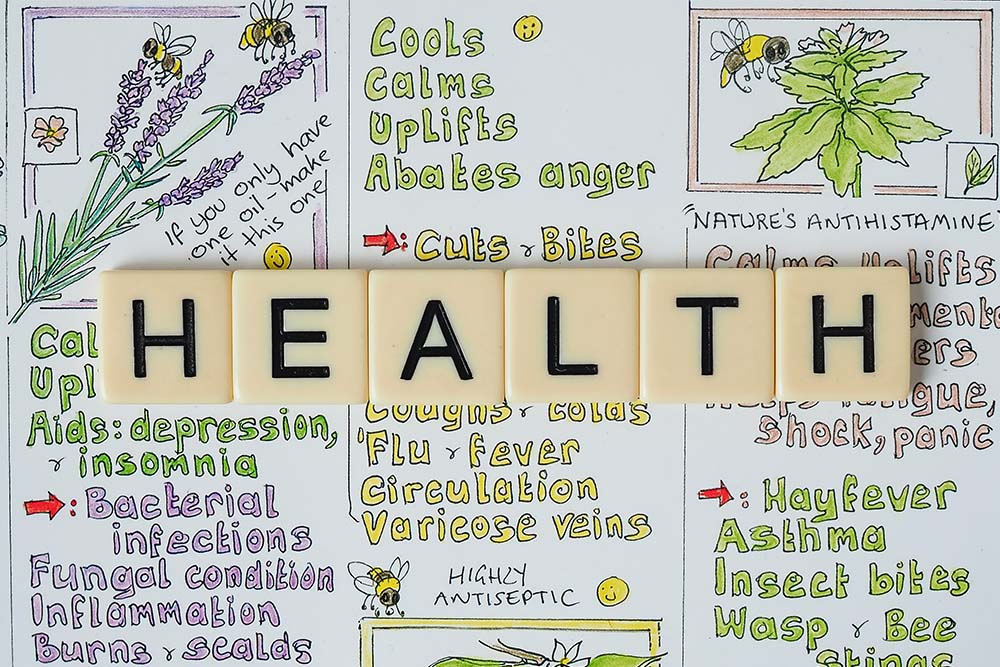
How the immune system plays a role in killing cancer
Every single day your immune system is fighting to defend your body from illness and infection. It is constantly battling against an invasion harmful pathogens, viruses, and bacteria, as well as the odd mutated cell that is set on destroying your body from the inside out.
With this in mind, your immune system should be able to kill off any nasty, hyper-proliferative cancer cells – but they don’t always.
For some reason, some tumours simply slip through the cracks.
While they are different from normal cells, they might share just enough similarities to avoid destruction. In some cases, they even develop ways of avoiding detection by your immune system – which is how they get so out of hand.
But what if we could change that?
Enter the T-cell.
What is the T-cell?
A T-cell is a type of immune cell that is found inside your blood (Miliotou, 2018).
The job of this particular cell is to scan your body and assess whether there is a threat that needs to be eliminated, or not.
How does it work?
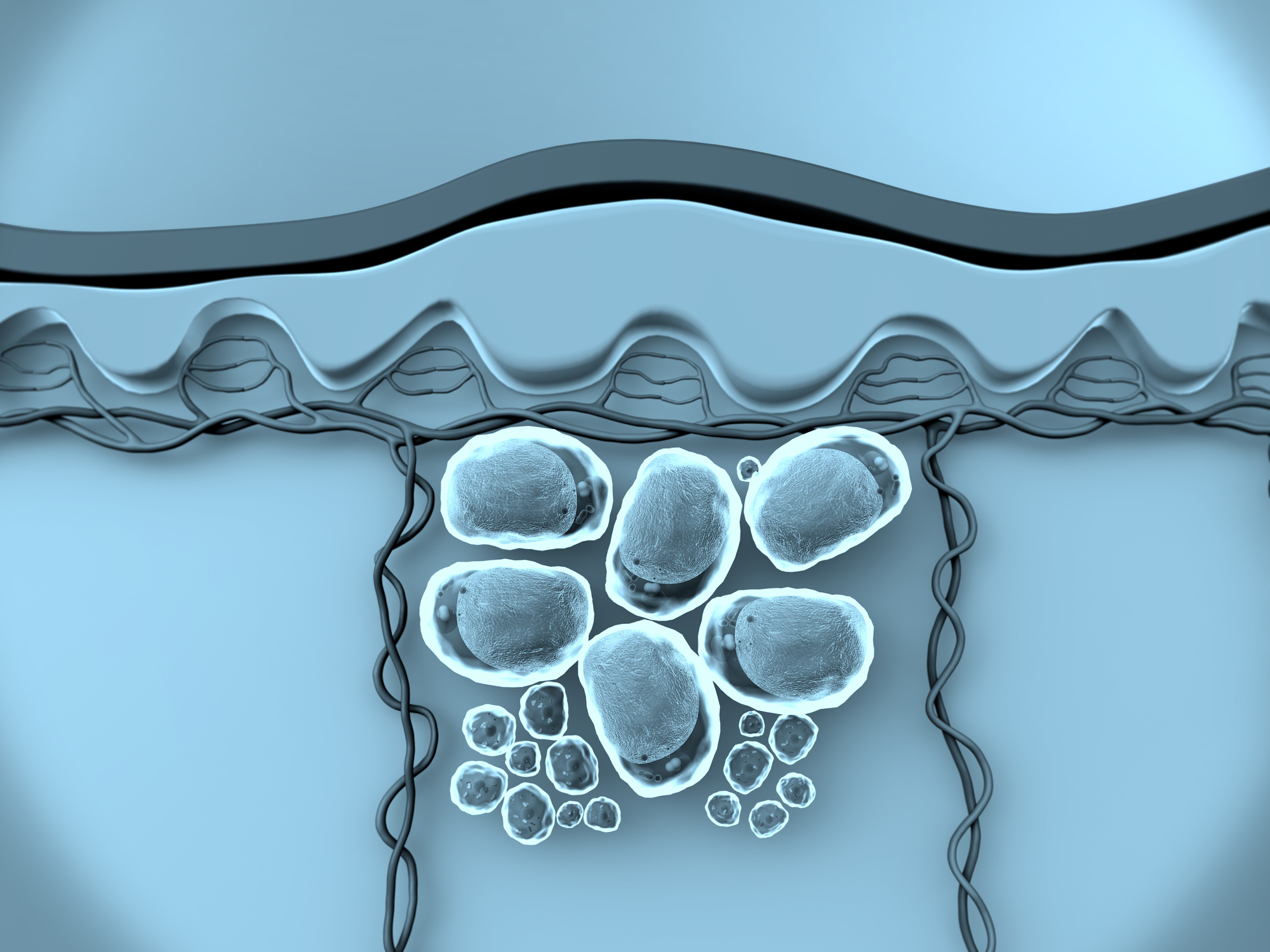
Well, very simply, T-cells have specific ‘receptors’ on their surface that allows them to ‘see’ at a chemical level. This allows them to distinguish between normal cells of the human body, and abnormal (or ‘cancerous’) cells.
While we all have T-cells in our body, there are different variations, with different receptors that have various degrees of efficiency – and this is where things start to get exciting.
A team of researchers from Cardiff university have discovered a T-cell and its receptor that can find and kill a wide range of cancerous cells in the lab – without harming any normal human cells in the process.
At this point in time it has shown promise when it comes to fighting lung, skin, blood, colon, breast, bone, prostate, ovarian, kidney and cervical cancer cells – and it is highly likely that it could be used to fight many more.
How would this work in practice?
I mentioned that this has shown a whole lot of promise in laboratory based studies – but that situation is markedly different from real life.
Firstly, a blood sample would need to be taken from the cancer patient. Their T-cells would then be extracted and genetically modified to contain the cancer-finding receptor discovered by the research team.
After which these upgraded cells would be grown in large amounts in the lab, before being put back into the patient.
This is a very similar process to a treatment known as CAR-T therapy, which uses a specific cancer fighting virus to alter the cells of the patient, rather than genetic modification.
When would it be tested and used on humans?
Given that this mode of treatment has shown so much promise in the lab, it is inevitable that it will eventually be trialled on humans.
Moreover, given the fact tat it is very similar to CAR-T therapy in application (which has been shown to be safe and effective), we already have the technology to implement it immediately.
However, we still have a way to go.
So far, this amazing cancer fighting procedure has only been tested in some animals, and on cells in the laboratory. As a result, way more safety checks would be needed before we could even think about starting a full blown human trial.
But hopefully we do start seeing them over the next couple of years.
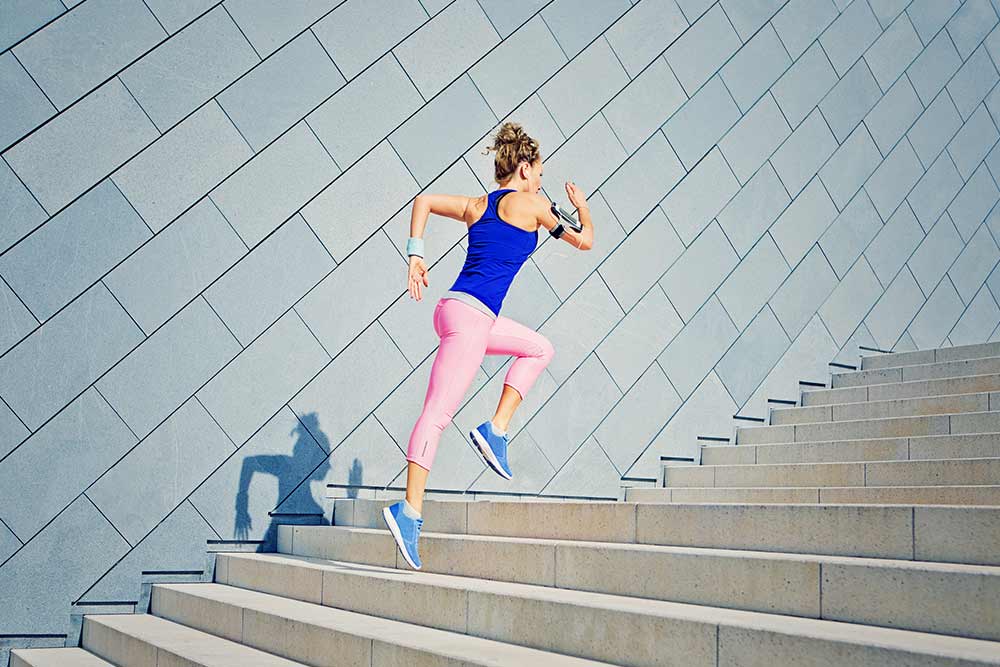
How exercise could complement treatment
In my opinion, one of the most exciting things about this new treatment comes down to the fact that it relies on the patient’s own immune system to do most of the fighting.
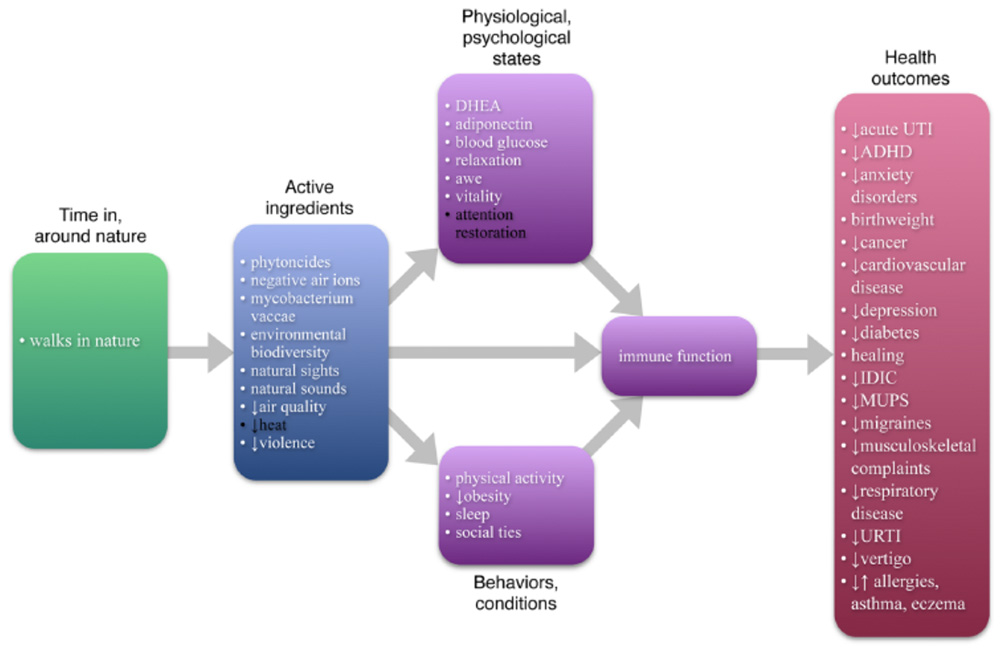
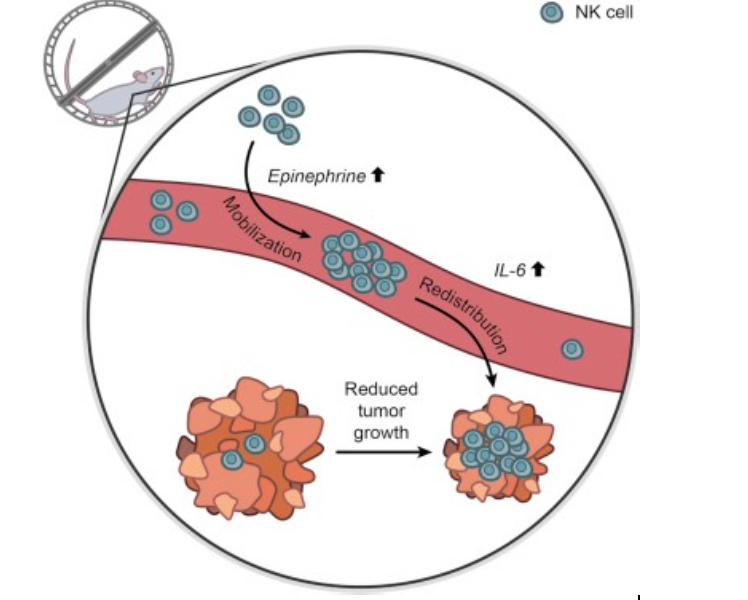
This means that exercising during treatment is likely to have a very positive effect (Nieman, 2019).
Exercise has been shown cause an increase in blood circulation throughout the body. This comes with an associated increase in the transport of immune cells throughout the body.
This increased immune cell circulation is then combined with a substantial increase in the secretion of anti-inflammatory cytokines, which lower inflammation throughout the entire body.
As a result, exercise has the potential to enhance immune system function – which is likely to enhance the effectiveness of treatment.
Yet, we obviously need to enter human trials before this is confirmed.
Related Article: Physical Activity and The Immune System
Where is the research is heading?
While the research into T-cell cancer therapy is only in its infancy, we have some very promising signs.
As such, it looks as if the next step is undertaking more animal based research to determine whether there are any nasty side effects associated with the treatment. If this is positive, then human trials won’t be far behind.
Finally, if this new treatment method appears to be safe and well tolerated in human participants, it can then be compared against more traditional treatment modalities to see how it shapes up.
Obviously, this is long way down the track, but that does not make it any less exciting.
Take Home Message
Given the terrible nature of cancer, any research breakthroughs are met with a lot of enthusiasm.
However, the excitement placed in this new T-cell treatment appears to be well founded. Especially considering just how many cancer cells it has killed off in the lab.
Now we just have to cross our fingers and hope that that future human trials show the same thing.
Related Article: Can Intermittent Fasting and Exercise Prevent Cancer?
References
Miliotou, Androulla N., and Lefkothea C. Papadopoulou. “CAR T-cell therapy: a new era in cancer immunotherapy.” Current pharmaceutical biotechnology 19.1 (2018): 5-18.
Nieman, David C., and Laurel M. Wentz. “The compelling link between physical activity and the body’s defense system.” Journal of sport and health science 8.3 (2019): 201-217.
You Might Like: