Autoimmune Illnesses: How To Move When Your Immune System Has Gone Rogue

Gillian White, MSc, Ph.D. (Candidate), University of Toronto, Graduate Department of Exercise Sciences
Autoimmune disorders – Rheumatoid Arthritis, Irritable Bowel Disease, Fibromyalgia, among others – represent a category of illnesses that are characterized by your immune system fighting your own cells. The symptoms specific to the different types of autoimmune diseases – joint damage and pain of Rheumatoid Arthritis, gut dysfunction of Irritable Bowel Disease etc. – are representative of the type of normal healthy cells in your body that your immune system is mistaking as an enemy and attacking. A hallmark of these illnesses is inflammation, which is usually the target of pharmaceutical interventions for these illnesses.
Autoimmune diseases are more common in women (about 2x higher) and emerge between the ages of 14 and 44 (Di Giuseppe et al., 2013). While no definitive cause has been identified, autoimmune diseases are likely related to both genetic predisposition (if other family members had/have it) and environmental factors. Importantly, lifestyle factors such as diet and exercise can have significant influence over disease progression and severity of symptoms and don’t produce the same side-effects as the prescription anti-inflammatories or steroids used to treat symptoms.
Related Article: Exercise & Celiac Disease
How Exercise Might Affect Autoimmune Diseases
Immunology-101
Your body has two types of immune cells: innate immune cells recognize things that are considered “non-self” (i.e. pathogenic viruses, bacteria etc.) and attempt to attack and kill the “non-self” entity. Specialized innate cells carry a little piece of the killed “non-self” invader back to the lymph nodes where it is used as a template for building an army of adaptive immune cells to identify and attack the “non-self” invaders. These adaptive immune cells are activated by pro-inflammatory signals released by innate immune cells and also attracted by these inflammatory signals to know where to attack. When they are activated, they release more pro-inflammatory signals so the inflammatory response snowballs, contributing to pain, swelling, and dysfunction of tissues (i.e. joints, gut, etc.).
While this is well and good when the “non-self” cell really is an invader, it’s extremely problematic when those “non-self invaders” are actually your body’s healthy cells. This is effectively what happens in an autoimmune disease. While it is not necessarily possible to teach your immune cells that these cells are indeed healthy cells of your own body, by minimizing inflammation – the signals activating and attracting immune cells to attack – can be targeted resulting in slower disease progression and improved symptoms, such as pain and function.
Related Article: How Fruits & Veggies Counteract Chronic Disease
Exercise Immunology-101
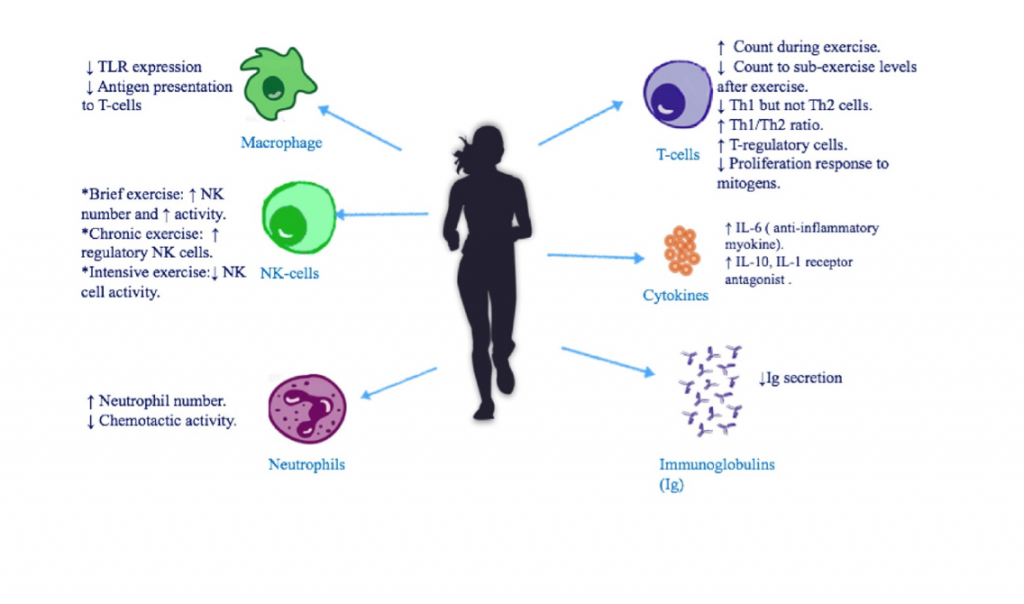
Figure 1. From Sharif et al. 2017 shows the immune effects of exercise. While exercise has an acutely pro-inflammatory effect (i.e. short-term), its chronic effects (long-term) are anti-inflammatory, helping to reduce rheumatic flare-ups and symptoms of auto-immune illnesses.
Exercise can influence the immune system, inflammation, and symptomology of autoimmune diseases in a number of ways (see figure 1). Firstly, regular exercise has anti-inflammatory effects resulting in lower chronic inflammatory status, which is related to disease progression and symptom severity. While the bout of exercise itself increases inflammation (~1 hour or so) it results in lower inflammation over the other 23 hours of the day. On balance, this is very beneficial for autoimmune sufferers. Exercise also seems to promote the shift of immune cells from a pro-inflammatory form attracted to clear cells (either non-self or damaged) to an anti-inflammatory from.
Steroids and Anti-inflammatory Drugs
While steroids and anti-inflammatory drugs can undoubtedly reduce inflammation and blunt immune system over-activation, they have unwanted side-effects such as:
- Weight gain
- Muscle loss
- Mood disturbance
- Increased risk of infection
- Puffiness
Exercise can effectively reduce chronic inflammation and associated symptoms as well as disease progression while also improving:
- Fitness
- Muscle strength
- Overall function
- Quality of life
- Psychological well-being
It is also important to note that these “side-effects” of exercise also reduce the risk of secondary diseases that are common in autoimmune diseases. For example, increased cardiovascular fitness for Rheumatoid Arthritis patients reduces their risk of heart disease, which is the cause of disease-related death in 40-50% of rheumatoid arthritis sufferers. Similarly, exercise can reduce the risk of ankylosing spondylitis in people suffering from Irritable Bowel Diseases, a common cause of pain and dysfunction in this population. Lastly, exercise improves psychological stress, which can cause flare-ups of symptoms and contribute to a poorer quality of life.
Related Article: Get Active With Rheumatoid Arthritis
Takeaway
Overall there are many reasons for people with autoimmune diseases to exercise. The following sections will investigate the research that has been done and the type of exercise that is best for Rheumatoid Arthritis, Irritable Bowel Disease, and Fibromyalgia. While these are only a few types of autoimmune diseases, exercise can be beneficial for all autoimmune diseases by improving inflammation and fitness resulting in better symptoms, function, and quality of life.
Related Article: Effect Of Gluten-Free Diet On Endurance Performance
You Might Like:
Everyday Tips To Be More Mindful
Gillian White – MSc, PhD (Candidate), University of Toronto Mindfulness Part II. Everyday tips to be more mindful. As I discussed in the previous article, Mindfulness Part I, the pursuit and practice of mindfulness has...The Jury Is Out | The Best Exercise for Parkinson’s Disease
Gillian White, MSc, PhD (C) University of Toronto, Graduate Department of Exercise Sciences Parkinson’s disease is a neurodegenerative condition affecting 2% of the population over 70 years of age – roughly 6 million people worldwide...Exercise Recommendations For Irritable Bowel Diseases
Gillian White, MSc, Ph.D. (Candidate), University of Toronto, Graduate Department of Exercise Sciences Irritable Bowel Diseases (IBD) include ulcerative colitis (UC) and Crohn’s Disease (CD) and are autoimmune diseases characterized by chronic inflammation of the...Is HIIT Beneficial For Rheumatoid Arthritis?
Gillian White, MSc, Ph.D. (Candidate), University of Toronto, Graduate Department of Exercise Sciences Rheumatoid Arthritis (RA) RA is an autoimmune disorder resulting in pain, swelling, and stiffness of joints and has been previously discussed in...Autoimmune Illnesses: How To Move When Your Immune System Has Gone Rogue
Gillian White, MSc, Ph.D. (Candidate), University of Toronto, Graduate Department of Exercise Sciences Autoimmune disorders – Rheumatoid Arthritis, Irritable Bowel Disease, Fibromyalgia, among others – represent a category of illnesses that are characterized by your...Exercise, Airways, and Sleep Apnea Prevention
Gillian White, H.BSc., M.Sc., PhD (C) University of Toronto, Department of Exercise Sciences As previously discussed in the recent “What’s keeping you awake” article, both acute and chronic exercise has been shown to improve sleep...- Arnold LM, Choy E, Clauw DJ, Goldenberg DL, Harris RE, Helfenstein M et al. (2016) Fibromyalgia and chronic pain syndromes: a white paper detailing current challenges in the field. Clin J Pain. 32(9):737-746.
- Bidonde JBA, Schachter CL, Overend TJ, Kim SY, Goes SM, Boden C, et al. (2017) Aerobic exercise training for adults with fibromyalgia. Cochrane Database Syst Rev.
- Busche AJ, Webber SC, Richards RS, Bidonde J, Shcachter CL, Shafer LA et al. (2013) Resistance exercise training for fibromyalgia. Cochrane Database Syst Rev. 12:Cd010884.
- Clauw DJ. (2014) Fibromyalgia: A clinical review. 311(15):1547-1555.
- Di Giuseppe D, Bottai M, Uitterhoeve R, van Riel P, can Achterberg T. (2015) Physical activity and risk of rheumatoid arthritis in women: a population-based prospective study. Arthritis Res Ther.17(1)
- Hoffman-Goetz L, Pervaiz N, Packer N, Guan J. (2010) Freewheel training decreases pro- and increases anti-inflammatory cytokine expression in mouse intestinal lymphocytes. Brain Behav Immune. 24(7):1105-1115.
- Khalili et al. (2013) Physical activity and risk of inflammatory bowel disease: prosp[ective study from the Nurses’ Health Study cohorts. BMJ [Br Med J].
- McBeth J & Mulvey MR. (2012) Fibromyalgia: mechanisms and potential impact of the ACR 2010 classification criteria. Nat Rev Rheumatol. 8(2):108-116.
- Persson P-G, et al. (1993) Risk indicators for inflammatory bowel disease. Int J Epidemiol. 22(2):268-272.
- Sharif K, Watad A, Bragazzi NL, Lichtbroun M, Amitral H, Shoenfeld Y. (2017) Physical Activity and autoimmune dieases: get moving and manage the disease. Autoimmun Rev. (in press)
- Sandstad J, Stensvold D, Hoff M, Nes BM, Arbo I, Bye A. (2015) The effects of high intensity interval training in women with rheumatic disease: a pilot study. Eur J Appl Physiol.115(10):2081-9.
- van West D, Maes M. (2001). Neuroendocrine and immune aspects of fibromyalgia. 15(8):521-531.










