Exercise Recommendations For Irritable Bowel Diseases

Gillian White, MSc, Ph.D. (Candidate), University of Toronto, Graduate Department of Exercise Sciences
Irritable Bowel Diseases (IBD) include ulcerative colitis (UC) and Crohn’s Disease (CD) and are autoimmune diseases characterized by chronic inflammation of the lining of the gastrointestinal system. UC affects the lining of the large intestine in which chronic inflammation can cause sores (ulcers) in this part of the digestive tract, while the chronic inflammation associated with CD affects the deeper tissues of the large intestine. Both can result in abdominal pain and cramping, diarrhea/constipation, blood in stool, and ulcers and can lead to more serious gastrointestinal complications including obstructed bowel, anal fissures, and colon cancer. Other more general symptoms include fatigue, unintended weight loss, bone mineral loss (osteopenia/osteoporosis), pain and swelling in eyes, joints, or skin, and malnutrition.
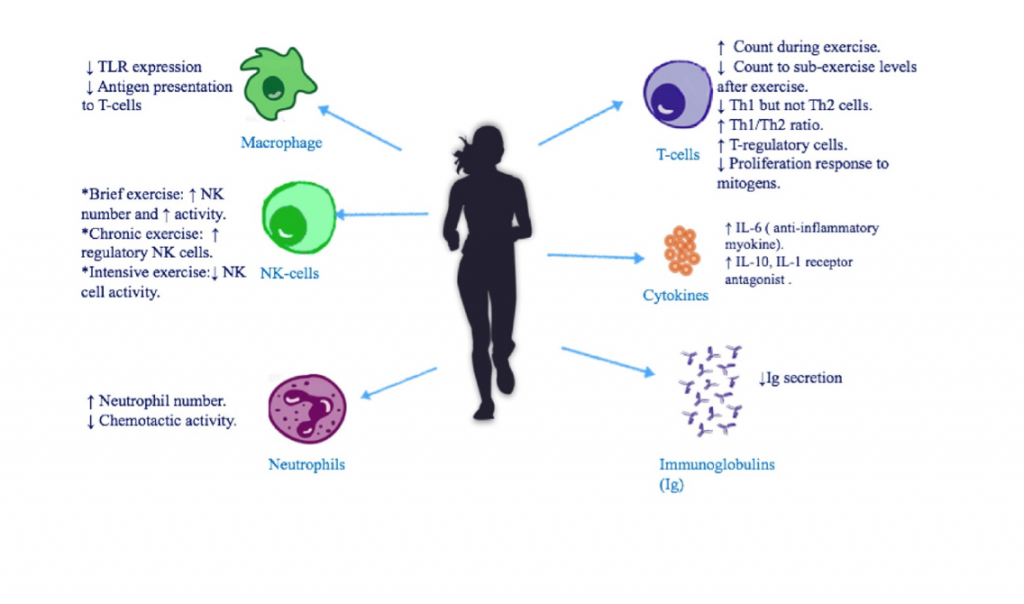
Figure 1. From Sharif et al. 2017 shows the immune effects of exercise. While exercise has an acutely pro-inflammatory effect (i.e. short-term), its chronic effects (long-term) are anti-inflammatory, helping to reduce rheumatic flare-ups and symptoms of auto-immune illnesses.
Physical Activity
Physical activity has been shown to reduce the risk of both UC and CD, although the effect is greater for CD (Persson et al.,1993; Khalili et al., 2013). Exercise can reduce disease progression and diarrhea symptoms, effects that are associated with lower pro-inflammatory signaling (Hoffman-Goetz et al., 2010). It may also reduce the risk of developing secondary illnesses associated with the primary IBD, such as ankylosing spondylitis, osteoporosis, and colon cancer. No studies have specifically measured the effects of exercise on pain, fatigue, or sleep quality in people with IBD but these symptoms in other autoimmune diseases tend to improve with regular physical activity.
Related Article: Autoimmune Illnesses: How To Move When Your Immune System Has Gone Rogue
Summary of Recommendations:
General Recommendations: >20 minutes of physical activity daily.
Best exercise: HIIT – 4×4 minutes x 85-95% HRmax with 3 minutes of rest at 70% HRmax done 2-3x/week.
Other exercise:
Aerobic – 25-35 minutes of moderate intensity aerobic activity (55-75% HRmax) done 3-4x/week
Resistance – 25-35 minutes of resistance training with progressive loads and focus on large muscle groups (i.e. lunges, squats etc.). Start with lower weight and higher repetitions (12-15 reps) for the first 4 weeks and gradually increases to higher weight with lower repetitions (8-10 reps).
Benefits: Lower pain symptoms, improved joint function, increased cardiovascular fitness, and lower risk secondary illnesses like heart disease (RA), osteoporosis (IBD), depression (Fibromyalgia). Track overall fitness improvements with a smart fitness watch!
Cautions: When fatigue is high, lower intensity aerobic exercise may be more suitable. A gentle routine on a yoga mat is recommended, for instance. For IBD, if surgical resection of intestines >10cm, high intensity exercise should be avoided.
Related Article: 4 Areas Of The Brain That Benefit From Exercise
You Might Like:
The Best Way to Prevent Gut Rot During Your Workout
Alyssa Bialowas One of the worst things that can happen to you before you start an intense workout, or worse as you’re 30 seconds into a run or a race: gut rot. Feeling pain and...Exercise Recommendations For Irritable Bowel Diseases
Gillian White, MSc, Ph.D. (Candidate), University of Toronto, Graduate Department of Exercise Sciences Irritable Bowel Diseases (IBD) include ulcerative colitis (UC) and Crohn’s Disease (CD) and are autoimmune diseases characterized by chronic inflammation of the...Exercise & Celiac Disease
Julia C. Basso, PhD Eating gluten free seems to be in fashion at the moment. You can find gluten free foods at almost every super market these days. However, for some gluten free is not...Exercise and Digestive Health
Julia Basso – PhD Dr. Shawn Khodadadian of Manhattan Gastroenterology writes that, “Exercise and digestion are mutually exclusive.” When you exercise, blood travels to your muscles and lungs (where it is needed) and away from...References:
- Arnold LM, Choy E, Clauw DJ, Goldenberg DL, Harris RE, Helfenstein M et al. (2016) Fibromyalgia and chronic pain syndromes: a white paper detailing current challenges in the field. Clin J Pain. 32(9):737-746.
- Bidonde JBA, Schachter CL, Overend TJ, Kim SY, Goes SM, Boden C, et al. (2017) Aerobic exercise training for adults with fibromyalgia. Cochrane Database Syst Rev.
- Busche AJ, Webber SC, Richards RS, Bidonde J, Shcachter CL, Shafer LA et al. (2013) Resistance exercise training for fibromyalgia. Cochrane Database Syst Rev. 12:Cd010884.
- Clauw DJ. (2014) Fibromyalgia: A clinical review. JAMA. 311(15):1547-1555.
- Di Giuseppe D, Bottai M, Uitterhoeve R, van Riel P, can Achterberg T. (2015) Physical activity and risk of rheumatoid arthritis in women: a population-based prospective study. Arthritis Res Ther.17(1)
- Hoffman-Goetz L, Pervaiz N, Packer N, Guan J. (2010) Freewheel training decreases pro- and increases anti-inflammatory cytokine expression in mouse intestinal lymphocytes. Brain Behav Immune. 24(7):1105-1115.
- Khalili et al. (2013) Physical activity and risk of inflammatory bowel disease: prosp[ective study from the Nurses’ Health Study cohorts. BMJ [Br Med J]. 347.
- McBeth J & Mulvey MR. (2012) Fibromyalgia: mechanisms and potential impact of the ACR 2010 classification criteria. Nat Rev Rheumatol. 8(2):108-116.
- Persson P-G, et al. (1993) Risk indicators for inflammatory bowel disease. Int J Epidemiol. 22(2):268-272.
- Sharif K, Watad A, Bragazzi NL, Lichtbroun M, Amitral H, Shoenfeld Y. (2017) Physical Activity and autoimmune dieases: get moving and manage the disease. Autoimmun Rev. (in press)
- Sandstad J, Stensvold D, Hoff M, Nes BM, Arbo I, Bye A. (2015) The effects of high intensity interval training in women with rheumatic disease: a pilot study. Eur J Appl Physiol. 115(10):2081-9.
- van West D, Maes M. (2001). Neuroendocrine and immune aspects of fibromyalgia. BioDrugs. 15(8):521-531.













