Sleep and Health – Sleep Series Part 3

Part 3 of Sleep Series – Sleep and Health
Sleep Stats and General Information – Sleep Series Part 1
Sleep Physiology – Sleep Series Part 2
We know that sleep is important for functioning and feeling energetic, but it is also an active contributor to our overall health. Our sleep and health are related! Hormones released during sleep decrease inflammation, fight free radicals, activate our immune system, and help organs rest and repair to keep them healthy and functional.
The central effect of sleep in maintaining health is in the imperative role it plays in maintaining a balance between our various stress systems. The HPA axis (cortisol), the autonomic nervous system (fight or flight responses), and inflammation are all impacted. These systems are activated to deal with day to day stressors and must be kept in balance to maintain health (see figure 1). When they’re turned on too high, they cause wear and tear on our organs, making us feel stressed and anxious. However, when they aren’t responsive, we can underreact to situations that require us to be vigilant.
This section of the Sleep Series will discuss the effects of sleep on brain health and function, cardiovascular health and weight management, and immune function.
Brain Health and Function
The impact sleep has on how we function is most obviously experienced in how our brain works. When we get a great sleep, we’re sharp, focused, productive, and can solve any problem with creativity and perseverance. When we don’t get enough sleep, we’re slow, distracted, irritable, and have a hard time staying on task, especially if that task proves challenging. The reasons for this lie in the important active processes of sleep. Namely, these are the removal of metabolic wastes during slow wave sleep, the formation of neuronal connections during REM sleep, and the release of hormones that keep inflammation and other stress hormones low.
Metabolic Waste Clearance
All animals require sleep, so it must be vital, but why is it so critical to life? An incredible study by Xie et al. in 2012 used photon-imaging in mice to uncover the mystery of sleep. They studied mice in waking states and sleeping or anesthetized states and found that the interstitial space around brain cells expands by 60%, which allows a greater exchange of wastes from within the cell with the cerebrospinal fluid moving around the cell. Basically, you can think of the brain cells shrinking to allow cerebrospinal fluid to wash over the brain cells, clearing them of wastes.
The waste product in question is called amyloid beta, which builds up in brains cells that are producing/using a high degree of metabolic energy (i.e. cells that are working hard). This build up interferes with the effective and efficient function of these cells, slowing conduction of neural transmission, thereby requiring more energy to be made for the same brain functions to occur. And hence, your brain doesn’t work so good. These amyloid beta proteins have also been implicated in the development and progression of cognitive decline during old age, including dementia and Alzheimer’s.
Asleep vs. Awake
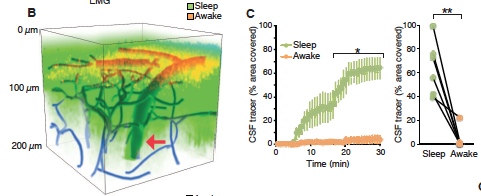
Figure 1. B. Shows the amount of area covered by cerebrospinal fluid (CSF) when asleep (green) compared with awake (yellow). C. Shows this same observation by percentage of area of the brain covered. This illustrates that more than 65% of the brain is covered during sleep, compared to less than 5% during wakefulness. This means that ~60% more volume of the brain is exposed to CSF, allowing the wastes to be removed from those cells. Xie et al; 2012.
Formation of Neural Connections
During REM sleep, the process of memory consolidation occurs, turning short-term memories formed during the day into long-term memories to be stored for the future. P-waves released from your pons (brain stem) during REM sleep activate your amygdala and hippocampus, which solidify memories (Datta et al. 2004). This is critical for learning processes to occur – when rats taught a maze pathway had REM sleep interfered with, they continued to struggle with the maze, while those who were allowed REM sleep undisturbed learned the path effectively (Datta et al. 2004). This goes for all kinds of learning: academic (hello, teenagers? Come in, teenagers?), occupational, sports – you name it, REM sleep is involved in remembering something that you know today, tomorrow.
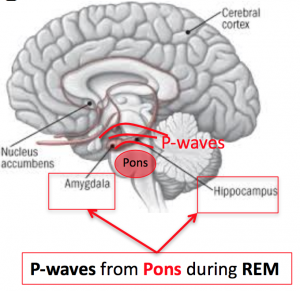
Figure 2. P-waves projected from the pons to the hippocampus and amygdala during REM sleep. These promote the formation of neural connections and memory consolidation that underlie the brain processes of learning.
Energy Repletion & Hormone Stabilization
Partial sleep deprivation is associated with reduced cerebral metabolism in the prefrontal and cortical brain regions (Kahn-Greene et al. 2007). These regions are critical for executive functions including goal setting, attention, focus, cognitive flexibility, and working memory. This seems like a lot of functions, and it is. Further, these functions are needed for everything from solving a problem at work, to sticking to deadlines, to coping with emotional stress, and eating vegetables for dinner instead of chips and wine (what? No, I didn’t).
Our ability to make good decisions relies on good executive function, so when there’s no fuel in the tank or when those parts of the brain are fatigued, we’re more likely to make bad decisions or quit when the going gets tough.
In the long term, this can have lasting effects because the brain’s structure and function is determined by a “use it or lose it” principle. Effectively, if we’re too tired to make good decisions, problem solve, regulate our emotions, etc. such that we are flexing these functions less and less, the brain networks that underlie those functions start to get rusty and become more difficult to activate.
Ultimately, we become our sleepiness-induced bad habits. Brain scans of people with chronic partial sleep or sleep disorders like sleep apnea show long-term restructuring of the brain – a long-term sleep deprivation maladaptation (Canessa et al. 2010). When our stress regulatory brain regions don’t work well or the neural pathways that regulate stress become overgrown, our body is more likely to stay in fight or flight mode, which has lasting health consequences.
Quick Facts
Brain function after acute partial sleep deprivation (<6h/night for days):
- Lower Attention
- Reduced Cognitive Performance
- Lower Emotional Regulation
- Mood Disturbance
- Lower Reaction Time
- Lower Motor Control & Coordination
- Impaired Working Memory
Brain function after chronic partial sleep deprivation (<6h/night for months – years):
- Structural Brain Changes
- Impaired Executive Function
- Impaired Emotional Regulation
- Poorer stress regulation (and associated health consequences)
Cardiovascular and Metabolic Health
Sleep doesn’t just make us feel rested but is actually considered by epidemiologists (people who study population trends in illnesses) to be a health imperative (Luyster et al. 2012). Everyone knows that being physically active is good for your cardiovascular health and helps promote a healthy body weight.
So, it may be counter-intuitive to discover that sleep – basically the opposite state of physical activity – is also good for your cardiovascular health and body weight. There is, of course limits to this. It’s not just “more sleep = more health.” However, very reliable evidence exists that partial sleep deprivation increases cardiovascular risk factors like hypertension and chronic inflammation. In addition, it impairs metabolic function resulting in obesity and diabetes.
Cardiovascular Health
A study of 5500 people reporting
When insufficient sleep becomes a habit, our body will spend more time than it should in an activated state, such that our vital organs don’t get the rest they need.
As shown in the figure below, an inverted-U pattern has been reported, in which <7h/night or >8h/night is associated with higher risk of hypertension (Luyster et al. 2012). While hypertension is an independent risk factor for cardiovascular disease, it’s not the only one affected by chronic sleep insufficiency. Excessive sympathetic activation results in chronic inflammation and immune stimulation, which is thought to be a significant risk factor in the development of cardiovascular disease (Faraut et al. 2012).
Inflammatory signaling contributes to lasting remodeling of the heart and blood vessels, and is another risk factor in cardiovascular disease and all-cause mortality.
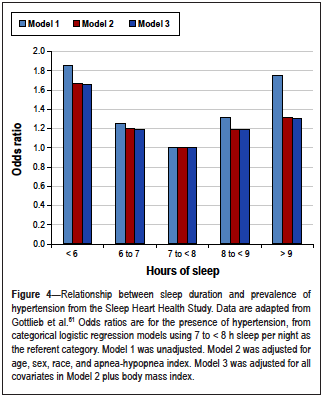
Figure 3. The likelihood of having hypertension according to average number of hours of sleep per night. Luyster et al.; 2012.
Obesity & Metabolic Function
A single night of partial sleep deprivation will make you inclined to eat more (Brondel et al. 2010). As shown in figure 4, an inverted-U relationship between both BMI (Taheri et al. 2004) and type II diabetes (Gotlieb & Punjabi, 2005) incidence exists for number of hours of sleep per night, similar to that for hypertension shown in figure 3. The astute reader may say, “well of course you’ll eat more – you’re awake for more hours, and therefore you will consume more calories.” However, a reader remembering that decision making is impaired may say, “no, your willpower is reduced, so you have lower self-control.”
While these are both probable contributors to the effects of sleep on metabolic regulation, the regulation of appetite hormones and metabolic hormones is an active process that occurs during sleep (Spiegel et al. 2004). Specifically, the hormones that make you feel hungry increase, while the hormones that make you feel full decrease. This adds up to you feeling hungrier (on average by 24%!), in addition to having lower self-control and more hours awake with the fridge (Spiegel et al. 2004).
Fluctuations of Cortisol
Other metabolic contributors to the relationship between sleep and obesity exist, including the fluctuations of cortisol. Cortisol is a stress hormones that stimulates glucose circulation in the blood and the metabolic pathways that use glucose for energy. When these are increased with no stress increasing the demand for glucose, it just stays in the blood or goes into storage mode. This is kind of like the boy who cried wolf. Eventually, the receptors that respond to cortisol, insulin, and blood glucose stop heeding the call and become less responsive. Ultimately, this leads to the dysfunctional glucose metabolism, known as insulin resistance, that underlies metabolic syndrome, type II diabetes, and obesity.
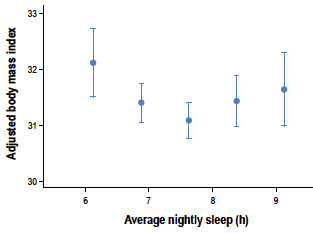
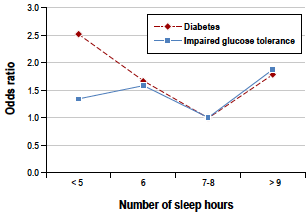
Figure 4. Inverted-U relationship between average hours of sleep and BMI. Roughly 7.7 relates to the lowest BMI. Taheri et al.; 2004. The odds ratio (likelihood) of experiencing diabetes of impaired glucose tolerance – a test for glucose metabolic function – according to average hours of sleep. Gotlieb & Punjabi; 2005.
Immune Function
Our immune system is comprised of two arms that work together: the innate immune system and the adaptive immune system. The innate system targets anything that it identifies as “non-self”, but to fight pathogens, it must randomly encounter them in the blood, or follow biomolecular signals released from another immune cell that’s already encountered the pathogen. While it has to depend on these random encounters to protect the body from would-be invaders, it has the benefit of acting immediately to neutralize the threat.
Conversely, the adaptive immune system is shown the specific patterns of the pathogen in question (more specific than just “non-self”). It creates an army of these cells ready to attack. And with the “picture” of the perpetrator, go hunting in the blood/body. While this is a more effective and targeted way of taking care of invaders, it takes a little longer to build and disseminate the army of cells. The innate system has enough fire power to keep the invader at bay until the adaptive system is trained and en route. But, eventually, it will lose out to the pathogen without the adaptive system’s action, resulting in infection and illness.
Sleep and Innate Immunity
During sleep deprivation, stress hormones increase (epinephrine, norepinephrine, cortisol) and anabolic hormones decrease (dopamine, prolactin, growth hormone) (Meerlo et al. 2002). Stress hormones can promote inflammatory signaling by activating NFkB, which controls inflammatory genes in the cells (Irwin et al. 2006). This is important because not only are these inflammatory markers signals for immune function, they are well-known risk factors for most chronic illnesses (cardiovascular disease, metabolic syndrome, diabetes) and mental illnesses (depression, chronic fatigue). High basal levels of inflammation also impair cognitive function, making your brain slow and foggy.
Studies using early night sleep deprivation (kept awake until 3am) have shown increased inflammation the next day, as well as reduced activity of Natural Killer cells. These are one of the innate immune system’s more important players (Irwin et al., 1994, 1996). Interestingly, females seem to take longer to recover from a night of sleep deprivation than males (Irwin 2010). But for most people catching up on sleep with a nap or extended sleep the next night will normalize innate immune impairments (Irwin, Carrillo, & Olmstead, 2010). It is important to note that inflammatory and innate immune changes are especially vulnerable to insufficiencies in slow wave sleep (Irwin 2008).
Since slow wave sleep happens more predominantly in the early part of the night, staying up late to finish a paper or report or to socialize with friends is the most likely type of partial sleep deprivation to impair immune function (Irwin et al. 1994, 1996).
Sleep and Adaptive Immunity
Melatonin, in addition to being a sleep regulating hormone, is also an anti-oxidant and immune regulator. In addition to promoting the release of growth hormone, it also scavenges free radicals and protects the cells’ mitochondria. These functions protect cells from damage, DNA dysfunction, and cell death – all of which contribute to a healthier brain and body.
Interestingly, the effects of a given stressor on adaptive immunity can be seen in their response to an immunization, since an immunization is basically doing the body’s job of showing the cells the “picture” of the “perpetrator” or pathogen ahead of actually coming into contact with it in the body. The adaptive system will make an army so it is ready to fight whatever pathogen it is trained to fight (i.e., flu, polio, TB, or whatever). It does this by producing antibodies that are specific to that pathogen. The more antibody produced, the stronger the adaptive immune system response.
Marginalized Sleep
Using this technique, Lange et al. 2003, show lower antibody production to Hepatitis A when participants were deprived of sleep after they got their Hep A shot (figure 5). This is because the promoting effects of melatonin on cells of the adaptive immune system is reduced, resulting in lower production of antibody, and greater likelihood of infection. It’s not surprising that studies have also shown a greater susceptibility to the common cold and respiratory tract infections (i.e. sore throat, cough) when sleep is marginalized (Wilder-Smith et al. 2013).
Interestingly, when your body is fighting an infection, you tend to spend more time in slow wave sleep (Madje & Krueger, 2005). This effectively puts your body in a state of high immune function to fight the infection. It also explains why quality sleep keeps us healthy and helps us recover.
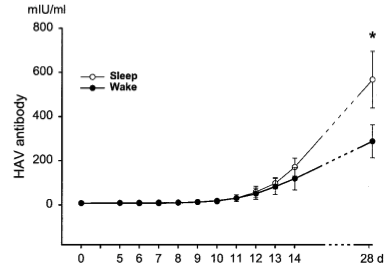
Figure 5. Antibody production in response to hepatitis A vaccination. The black line indicates antibody production when immunization was followed by sleep deprivation, compared with the white control line. Lange et al.; 2003.
Quick Tips
- Don’t sacrifice early night sleep (10pm-3am). This is when you get most of your slow wave sleep and is essential for a healthy immune system. It’s better for your health to go to sleep and wake up early to complete any work from the previous night.
- If you feel yourself coming down with something, prioritize early night sleep to give your immune system the time and support it needs to fight off whatever illness is trying to get you down.
- Women take longer to recover from sleep deprivation – so go ahead and put your feet up or take a nap! It’s better to steal a couple hours of extra sleep than be down for the count with a flu or cold for days or even weeks.
Bringing It All Together
Consequently, the effects of poor sleep habits have long-term effects on your health. This includes brain structure changes, which promote stress reactivity and illness processes related to stress. During this state, our autonomic system chronically activates and our organs that work all day don’t get the necessary time to rest, repair, and recover for the next day’s work.
Hence, this can contribute to psychological illnesses (depression), cognitive illnesses (dementia), cardiovascular illnesses (hypertension), metabolic illnesses (diabetes & obesity), and immunosuppression (cancer & viral/bacterial infections).
Overall, not only is your productivity and physical competency suffering, but your risk of illness and all-cause mortality (aka. “death”) increases! We’re far too quick to sacrifice sleep to make time for other things that we consider to be more important. But just because sleep doesn’t require effort, doesn’t mean it isn’t an active process that is essential for our body’s function, health, and happiness.
(adsbygoogle = window.adsbygoogle || []).push({});
You Might Like:
RFK’s Plan to Make America Healthy Again: A Vision for a Healthier Future
Robert F. Kennedy Jr. (RFK Jr.), a prominent environmental lawyer and political activist, has emerged as a voice for change in the United States. Known for his work on environmental and public health issues, particularly...The Science of Temperature Therapy
Temperature therapy (also known as “thermal therapy” or “thermotherapy”) involves the use of heat or cold to improve health and function. Interestingly, thermotherapy has been around for centuries, with ancient cultures regularly using hot springs,...The Predictors of Longevity You Need to Care About
Living a long and healthy life is a universal aspiration, and with the publication of Peter Aittia’s new book “Outlive”, it has never been a bigger focus. With this has come the realisation that, while...How Overtraining and Undertraining Impacts Hormonal Health
While maintaining a healthy hormonal balance is essential for overall health and wellbeing, it is an often-overlooked component of women’s health. Hormones play a vital role in regulating various bodily functions, including metabolism, energy, mood,...12 days of Fitness: 12 Holiday workouts to crush this Christmas
The holiday period is a time for friends, food, and family. With this in mind, it should be a time of guilt-free fun. However, that doesn’t mean you have to neglect your fitness entirely over...Upper Body Strength in Post-Menopausal Women
Menopause is a unique time in the human life, and with it comes a myriad of changes that can have wide reaching health implications. However, over the last 20 years we have seen a strong...References:
Brondel L1, Romer MA, Nougues PM, Touyarou P, Davenne D. (2010). Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr. 91(6):1550-9.
Canessa N, Castronovo V, Cappa SF, Aloia MS, Marelli S, Falini A, Alemanno F, Ferini-Strambi L. (2011). Obstructive sleep apnea: brain structural changes and neurocognitive function before and after treatment. Am J Respir Crit Care Med, 183(10):1419-26.
Datta S, Mavanji V, Ulloor J, Patterson EH. (2004). Activation of phasic pontine-wave generator prevents rapid eye movement sleep deprivation-induced learning impairment in the rat: a mechanism for sleep-dependent plasticity. J Neurosci. 11;24(6):1416-27.
Gottlieb DJ, Punjabi NM, Newman AB, et al. (2005). Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Int Med, 165:863-7.
Faraut B, Boudjeltia KZ, Vanhamme L, Kerkhofs M. (2011). Immune, inflammatory and cardiovascular consequences of sleep restriction and recovery. Sleep Med Rev.
Irwin MR, Carrillo C, Olmstead R. (2010). Sleep loss activates cellular markers of inflammation: sex differences. Brain Behav Immun, 24(1):54-7.
Irwin M, Mascovich A, Gillin JC, Willoughby R, Pike J, Smith TL. (1994). Partial sleep deprivation reduces natural killer cell activity in humans. Psychosom Med, 56(6):493-8.
Irwin M, McClintick J, Costlow C, Fortner M, White J, Gillin JC. (1996). Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. FASEB J, 10(5):643-53.
Irwin MR, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med, 166(16):1756-62.
References cont.:
Kahn-Greene ET, Killgore DB, Kamimori GH, Balkin TJ, Killgore WD. (2007). The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Med. 8(3):215-21.
Lange T, Perras B, Fehm HL, Born J. (2003). Sleep enhances the human antibody response to hepatitis A vaccination. Psychosom Med, 65(5):831-5.
Luyster FS1, Strollo PJ Jr, Zee PC, Walsh JK. (2012). Sleep: A Health Imperitive. Sleep. 1;35(6):727-34.
Majde JA, Krueger JM. (2005). Links between the innate immune system and sleep. J Allergy Clin Immunol, 116(6):1188-98.
Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. (2005). Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol, 99:2008-19.
Taheri S, Lin L, Austin D, Young T, Mignot E. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med, 1:e62.
Wilder-Smith A1, Mustafa FB, Earnest A, Gen L, Macary PA. (2013). Impact of partial sleep deprivation on immune markers. Sleep Med, 14(10):1031-4.
Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O’Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M. (2013). Sleep drives metabolite clearance from the adult brain. Science. 342(6156):373-7.
(adsbygoogle = window.adsbygoogle || []).push({});