The Autoimmune Athlete

Hunter Bennett
Being an elite athlete poses a unique set of challenges that very few people are emotionally, physically, and mentally prepared for. Gruelling training sessions, an incredibly strict diet, and a lifestyle that is dictated entirely by the competitive season.
It is a life that many people desire, yet many would also agree is in some ways very undesirable.
And it is made even more so by autoimmune disorders.
Enter the autoimmune athlete.
What are autoimmune disorders?
Autoimmune disorders are a unique type of condition in which your own immune system starts to attack your own body.
Sounds bad?
Well, that’s because it is.
Or rather, it can be.
Diving into this into a little more detail, the role of your immune system is to help protect your body from any invading pathogens. Under normal circumstances, it senses these invaders and sends out immune cells to destroy them.
Note that I said under normal circumstance.
You see, this isn’t the case with people who suffer from an autoimmune disorder.
If you have an autoimmune disorder, your immune system mistakes parts of your body as invaders. It then releases immune cells into that are of your body to kill off those tissues. In turn, this can lead to tissue damage, declines in health, and of course illness.
With all this in mind, it is important to note that not all autoimmune disorders are created equal. Some may only affect a single organ, others may only impact upon certain types of tissues (such as your joints), while others impact your entire body.
Some of the most common autoimmune disorders include: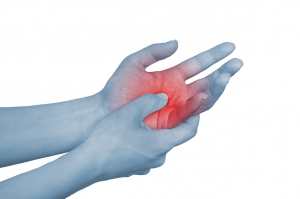
- Celiac disease
- Irritable bowel syndrome
- Lupus
- Rheumatoid arthritis
- Type I diabetes
In an athlete, any type of autoimmune disorder can be seriously damaging because it can impair their ability to train, recover, and perform.
Which is why recognizing the signs of an autoimmune disorder early is so damn important.
Related Article: Can I Exercise With An Overactive Thyroid?
What are the signs of autoimmune disorder in an athlete?
Taking this into consideration, some of the more common signs of autoimmune disorders include:
- Low energy, and sensations of mental and physical fatigue
- Sore and aching muscles
- Inflammation, swelling, and redness of the limbs, hands, and feet.
- The onset of a minor fever
- Difficulty concentrating and maintaining attention
- Numbness and tingling in the hands and feet
- The onset of hair loss
- The development of rashes on the skin.
When discussing symptoms, it is also very important to be aware that some specific autoimmune diseases can also have their own unique signs. For example:
- Type I diabetes can cause thirst and weight loss.
- Irritable bowel syndrome can belly pain, bloating, and diarrhea.
Additionally, with many autoimmune disorders, symptoms may simply come and go. In this manner, a period of more severe symptoms is commonly known as a flare-up, which is normally driven by an acute increase in inflammation.
Can exercise induce an autoimmune disorder flare up?
Now in my mind, this is where things get a little bit interesting.
There is evidence to suggest that long-term exercise helps reduce inflammation and improve immune system function. This can help prevent the development of an autoimmune disorder and assist in its treatment (Sharif, 2018).
But, as I have already alluded to, some people also flare up in response to stress (Stojanovich, 2008).
And exercise is a very specific type of stress…
With this in mind, some individuals may experience a flare-up after exercising. This is what we would normally consider being an exercise-induced autoimmune flare up.
It is also important to note that these type of flare-ups may be more likely to occur during times when stress is high in all aspects of life (think family stress, work stress, and even relationship stress), and recovery is simultaneously poor.
In this scenario, the athlete is most likely pushing themselves too hard while in a state of under-recovery, which can cause an increase in inflammation, and finally, a flare-up.
I should note that with all of this, athletes tend to tolerate exercise better than people from the general population. After an acute bout of exercise, they only see minimal increases in inflammation, and only very mild changes in immune system function (Lee, 2017).
This ultimately means that the fitter you are, the less likely you experience an exercise-induced autoimmune flare up.
What does an autoimmune flare feel like?
To put it very simply, a flare-up will feel like the normal symptoms of your autoimmune disease, albeit more severe. These symptoms should then fade away after a prolonged period of recovery, in which inflammation returns to normal.
For example, if a sign of your autoimmune disorder is mild tiredness and lethargy, you might feel completely exhausted and lacking all energy during a flare-up.
How to manage training with an autoimmune disorder
As I am sure you can imagine, training with an autoimmune disorder can become a little bit of a balancing act. The stress caused by exercise may be enough to induce a flare up, if the bout of training is extremely intense.
This means that you really need to regulate your training in accordance with how you feel.
If you are feeling good, your symptoms are minimal, and your recovery has been on point, then you are going to be in a prime position for a heavier block of training. Alternatively, if you are tired, run down, and dealing with some emotional stress, then a couple of light recovery days are probably in order.
This process doesn’t have to be very complex, but it does require you to listen to your body and respond accordingly.
Endurance training and autoimmune disorders
It is pretty darn obvious that almost every single athlete on the planet needs a well-developed aerobic system. It is this aerobic capacity that not only allows them to compete at a high level during a game but in the case of field athletes, also recover between intense bouts of activity.
Like I said – it is important.
Now, endurance training with an autoimmune disorder is pretty straightforward. Low and moderate intensity physical activity (think below 70% of maximal heart rate) only elicits a small increase in inflammation (Lira, 2017).
I should note that this increase is still somewhat dictated by the duration of exercise, so the longer you exercise, the greater that increase in inflammation will be – however, in the grand scheme of things, it will still be quite minimal.
The thing to really consider here is the mode of exercise.
Which is why running and autoimmune disorders are not always a great match.
You see, because running involves high impact forces each time your foot contacts the ground, it places quite a bit of load on your joints and muscle tissue. This load can increase muscle damage, which can increase inflammation (Nieman, 2014).
With this in mind, if you are feeling worn down but still need to complete some aerobic exercise, cycling or swimming may be a better option.
HIIT and autoimmune disorders
High-intensity interval training (HIIT) is one of the most effective ways of implementing exercise on the planet. It has been shown to cause vast improvement in both fitness and health, albeit in a very short amount of time.
But it does come at a bit of a cost.
Because it is performed at a much higher intensity than traditional steady-state aerobic exercise, it also increases inflammation more than lower intensity options (Cullen, 2016).
Now, this is not to say that athletes with an autoimmune disorder should never perform HIIT. In fact, in most scenarios, they will probably have to, as it can have a huge impact on their ability to perform both aerobically and anaerobically.
However, athletes with autoimmune disorders may want to save their HIIT session for those periods of time where they are feeling really good, and avoid it during times of fatigue.
They may also want to use easier modes of intensity (like rowing and cycling) for their HIIT sessions to further reduce the risk of developing a flare-up.
CrossFit and autoimmune disorders
Given the rise of CrossFit over the last decade, I thought it would also be important to discuss where it sits in the routine of someone suffering from an autoimmune disorder.
The thing to realize here is that CrossFit essentially combines high-intensity interval training with higher rep weight training and jumping and landing tasks.
To put it simply, it is a recipe for increasing inflammation as fast as humanly possible (Tibana, 2018).
To be clear, I am not denying the fact that it offers a very powerful way of improving muscular endurance, aerobic fitness, strength, and power, all simultaneously – because I am not.
All I am saying that if you are an athlete with an autoimmune disorder, you might be better spending your time elsewhere, and breaking up your training in a more manageable way.
Tips to manage autoimmune disorders in athletes
I have already stated that autoimmune disorders are very much driven by an increase in inflammation. This increase in inflammation essentially takes the body out a normal state of homeostasis, which exacerbates the disorder even further.
As such, I wanted to provide some tips for athletes with autoimmune disorders that offer a way to help reduce inflammation in the most effective way possible.
Diet to manage autoimmune disorders in athletes
The first point of call is to eat a healthy diet.
This means eating a diet that consists of mostly vegetables, whole fruits, whole grains, low-fat dairy, and a variety of protein dense foods, including seafood, lean meats and poultry, eggs, legumes (beans and peas), as well as nuts, seeds, and soy products.
With this, you should also try and limit your consumption of saturated fats, trans fats, added sugars, and sodium as much as possible (this means minimizing your intake of junk foods and sugary beverages).
You can also aim to consume foods that have specific anti-inflammatory properties, such as turmeric, seafood, and berries.
Finally, you also want to make sure that you are eating enough food to meet your energy demands.
This means eating enough high-quality carbohydrates to fuel your training sessions and eating enough protein to recover from those training sessions.
Sleep to manage autoimmune disorders in athletes
From a recovery perspective, sleep is hands down the most important thing you can give your body.
Poor sleep quality and inadequate sleep duration have both been shown to cause large and significant increases in inflammation, which can further exacerbate the signs and symptoms of an autoimmune disease (Simpson, 2007).
So, the key is to make sure you get enough good quality sleep every night – which can be done by using the following tips:
- Eliminate electronic screens for the hour immediately before bed
- Get a good sleep routine and go to sleep the same time every night
- Allow yourself at least 8 hours of sleep every night
- Avoid drinking caffeine after 2pm
Simple and effective.
Related Article: Exercise & Celiac Disease
Meditation to manage autoimmune disorders in athletes
Lastly, I wanted to touch on mindfulness and meditation.
You now know that all types of stress can contribute to inflammation and reduce immunity. Which is why finding ways to limit this inflammation is paramount to keeping your autoimmune disorder at bay.
There is a growing body of evidence to suggest that actively participating in meditation daily can improve mood, reduce stress, cause physical reductions in inflammation, and even improve immune system function (Black, 2016).
So simply commit to 10 minutes per day, and reap all the rewards.
Famous athletes with autoimmune disorders
Last but not least, I wanted to give you a clear demonstration that an autoimmune disease does not mean the death of your athletic career.
In fact, a number of high-profile athletes have had very successful careers while carrying an autoimmune disorder and were able to manage them through the use of diet and exercise.
These athletes include:
- Venus Williams: who has a rare autoimmune disease known as Sjogren’s syndrome, which causes severe muscle and joint pain.
- Phil Mickelson: has psoriatic arthritis, which is a unique type of autoimmune disease that can severely damage the body’s joints.
- Caroline Wozniacki: suffers from rheumatoid arthritis, an autoimmune disorder that attacks the joints of the body.
- Sandy Koufax: also suffered from rheumatoid arthritis for the entirety of his career.
While this is just a snapshot of the athletes who suffer from autoimmune dysfunction, take solace in the fact that they made it to the top level – and therefore so can you.
Take Home Message
Autoimmune disorders can be seriously debilitating.
They can cause some nasty physical side effects. They can make you feel tired and lethargic, and they can really make exercise a challenge. Which is why tailoring your training routine to both your needs and to how you feel is paramount.
The tips outlined in this article can be used to help fight the symptoms of autoimmune disorder so you can keep training and stay at the top of your game – so give them a go and let us know what you think.
References
Stojanovich, Ljudmila, and Dragomir Marisavljevich. “Stress as a trigger of autoimmune disease.” Autoimmunity reviews 7.3 (2008): 209-213.
Sharif, Kassem, et al. “Physical activity and autoimmune diseases: Get moving and manage the disease.” Autoimmunity reviews 17.1 (2018): 53-72.
Lee, Elaine C., et al. “Biomarkers in sports and exercise: Tracking health, performance, and recovery in athletes.” Journal of strength and conditioning research 31.10 (2017): 2920.
Lira, Fabio Santos, et al. “Short-term high-and moderate-intensity training modifies inflammatory and metabolic factors in response to acute exercise.” Frontiers in physiology 8 (2017): 856.
Nieman, David C., et al. “Immune and inflammation responses to a 3-day period of intensified running versus cycling.” Brain, behavior, and immunity 39 (2014): 180-185.
Cullen, Tom, et al. “Interleukin-6 and associated cytokine responses to an acute bout of high-intensity interval exercise: the effect of exercise intensity and volume.” Applied physiology, nutrition, and metabolism 41.8 (2016): 803-808.
Tibana, Ramires A., et al. “Corrigendum: Two Consecutive Days of Extreme Conditioning Program Training Affects Pro and Anti-inflammatory Cytokines and Osteoprotegerin without Impairments in Muscle Power.” Frontiers in physiology 9 (2018).
Simpson, Norah, and David F. Dinges. “Sleep and inflammation.” Nutrition reviews 65.suppl_3 (2007): S244-S252.
Black, David S., and George M. Slavich. “Mindfulness meditation and the immune system: a systematic review of randomized controlled trials.” Annals of the New York Academy of Sciences 1373.1 (2016): 13-24.